LOCATION
340 East 1st Avenue, Suite 333 Broomfield, CO 80020
PHONE
720-446-8675
BUSINESS HOURS
- Mon - Fri
- -
- Sat - Sun
- Closed
7,000+ Treatments Completed
More Conditions Treated With TMS
TMS Therapy for PTSD
Severe trauma engenders a range of extreme physical and psychological reactions. PTSD occurs in approximately 20% of victims of trauma and TMS may offer a return to normality.
-
What is Post Traumatic Stress Disorder?
Post Traumatic Stress Disorder-PTSD, is a psychiatric condition that follows a direct or indirect traumatic event. It typically presents with a number of problematic symptoms to be reviewed in more detail below and a chronically heightened stress state. Problems with mood and anxiety regulation occur and the mind and body struggle to reset and stay out of a fight or flight mode. Many of the symptoms of PTSD would be expected and normal in a life-threatening situation, but not in everyday life.
PTSD is most often associated with service personnel or veterans who have experienced active-duty combat and associated traumatic experiences. PTSD can occur in many other situations as well, however. Trauma can occur in small doses over many years or from one traumatic event. It can stem from things like abuse, an assault, or an accident. Some 7-9% of all people will experience PTSD in their lifetimes.¹
-
What causes PTSD?
When experiencing a real or perceived life-threatening situation, the brain will shift into ‘reptilian brain,’ prioritizing pure instinct and survival. It enters into the fight or flight mode and activates basic brain structures that keep the brain in a heightened sense of awareness and safety.
Once the threat has passed, the brain will typically down-regulate itself and return to its everyday default mode. Depending on the severity and repetitiveness of the stressful trauma, however, and the genetic predisposition of the individual, this may not occur effectively. Similar to circuits that become stuck and dysfunctional in clinical depression, certain pathways become fixed in a fight or flight response in PTSD.
-
Who is at risk of PTSD?
We all have different reactions to stressful and traumatic events and anyone can develop PTSD depending on the circumstances. Increased risk factors include:
Recurrent or longer-lasting trauma.
Suffering a physical injury or threat to life during trauma.
Lack of a support network.
Concurrent stress factors such as financial issues, homelessness, bereavement, or imprisonment.
History of depression and anxiety disorders.
Experiencing trauma in childhood.
Working in emergency services.
Refugee status.
-
Symptoms of Post Traumatic Stress Disorder - PTSD
The aftermath of a potentially life-threatening incident or repeated trauma typically manifests with natural reactions such as brief confusion, dissociation from one’s surroundings, exhaustion, a feeling of numbness, or acute anxiety or agitation. These expected reactions can support mental recovery and typically fade away. Continuing to struggle with symptoms to follow, however, indicate PTSD. PTSD symptoms have four distinct clusters:
Intrusive thoughts:
Flashbacks
Nightmares
Distressing memories.
Acute distress psychologically or physiologically at triggering reminders.
Negative mood and cognitions
Dissociative Amnesia - inability to recall aspects of the trauma.
Persistent negative emotions such as fear, anger, guilt, and/or shame.
Inability to experience positive emotions.
Feeling detached or estranged from surroundings and others.
Negativity and symptoms similar to depression such as lack of interest in activities.
Hypervigilance
Agitation and aggression.
Reckless or self-destructive behavior.
Startle response with panic attacks.
Insomnia
Difficulty concentrating.
Avoidance
Repeated effort to avoid memories or triggers related to the trauma.
Research has shown the brain actually changes biologically following traumatic experiences. Three significant brain areas become ‘dysregulated’ in PTSD:
The amygdala, responsible for recognizing and responding to threat, as well as attaching emotion to memory, becomes overactive and remains in an emergency and hypervigilant state.
The hippocampus, responsible for cells supporting neural connections that embed memory, shrinks. In reaction to the amygdala’s hypervigilance, stress hormones destroy the formation of new cells and memories that would ordinarily confirm that the threat has passed, solidifying the ‘high alert’ or reactive mode.
An area labeled the ventromedial prefrontal cortex no longer inhibits the hyperactive amygdala, thus reinforcing the inability of the hippocampus to form new memories and distinguish emotions connected to past from present.
Unsurprisingly, a combination of any of the above symptoms can severely interfere with everyday activities resulting in:
Low self-care.
Difficulties with performing and retaining a job.
Conflict in relationships and friendships.
Inability to make decisions.
Memory problems.
Struggling to deal with change.
Loss of simple joys and pleasure in life.
Inability to make decisions.
Furthermore, PTSD often occurs or causes parallel mental health issues such as:
Depression and anxiety disorders.
Suicidal ideation and/or self-harm.
Dissociative disorders.
Substance abuse.
-
Treating PTSD
Similar to other psychiatric conditions such as Major Depressive Disorder, the mainstay of treatment for PTSD involves medications and specific types of therapy. Therapy typically involves common approaches such as CBT (cognitive behavioral therapy) or more targeted therapy such as EMDR (eye movement desensitization and reprocessing), CPT (cognitive processing therapy), or exposure therapy. As is the case with Major Depression, however, PTSD treatment can often be resistant to these approaches. A recent meta-analysis showed that less than half of patients receiving trauma focused therapy achieved a meaningful response to treatment, some two-thirds of patients failed to achieve remission, and one-third dropped out of treatment. And the effect size for medications was even less than for therapy.²
TMS offers a unique approach and compelling results in the treatment of PTSD. Numerous studies have shown TMS to be an effective treatment option for PTSD when medications and therapy have not worked. Different protocols have been utilized in an attempt to treat the core symptoms of PTSD, but most, similar to depression treatment, also target an area of the brain called the dorsolateral prefrontal cortex. This area on the surface of the brain is involved in regulating deeper brain structures and can affect key areas of the brain that are involved in PTSD symptoms such as the amygdala and hippocampus.
What do the studies show?
Research has been going on for quite some time with TMS treatment for PTSD. A meta-analysis from 2014 summarized that TMS treatment for PTSD was effective and that the effect size was similar to TMS treatment for Major Depression.³ Studies reviewed included RCTs (randomized controlled studies) - the gold standard for research - and utilized validated rating scales for PTSD such as the PCL-5 (PTSD checklist) and the CAPS-5 (clinician administered PTSD scale). Some of the studies utilized as few as 10 treatments in two weeks and were found to be beneficial, but more sessions and more pulses per session tended to show greater improvement in symptoms.
More recent meta-analyses reviewing TMS treatment for PTSD have found similar and even more robust findings.⁴⁵⁶ RCTs have consistently shown at least one-third of patients with improvement on PTSD rating scales and others have been closer to one-half of patients experiencing significant response. Longer term response data is more limited, but points to at least 2-3 months of sustained response following treatment and a more recent paper has found benefit with TMS up to 1 year post treatment.⁷
In 2021, the VA implemented a nationwide study to evaluate clinical outcomes in veterans being treated with TMS.⁸ While the primary inclusion criteria for this study was Major Depression, around 68% of the patients in this study also suffered from comorbid PTSD, and both Major Depression and PTSD responses were measured. Of the 340 veterans with comorbid PTSD, 65.3% showed response and 46.1% no longer met threshold criteria after receiving an adequate dose of TMS.
Read more: TMS success rate →
Another study, which examined TMS as a monotherapy for PTSD and compared a 1 Hz protocol to a 10 Hz protocol, also found clinically significant improvements in PTSD symptoms after 30 TMS treatments.⁹ This study utilized multiple rating scales to evaluate response and remission results, and they found that around 29-46% of patients experienced response and 21-33% experienced remission (depending on rating scale). In addition to these findings, they also saw that both the 1 Hz and 10 Hz groups showed similar improvements in both PTSD and depressive symptoms, and these improvements were sustained at a 3 month follow up.
As listed above, a number of studies have shown very good results with TMS. It is not currently FDA approved for the treatment of PTSD, but often utilized off-label as PTSD can frequently be treatment resistant. As noted, other psychiatric conditions also commonly co-occur with PTSD. Major Depression occurs in some half of all PTSD sufferers. In light of this, additional treatment protocols that target PTSD more specifically can often be added into TMS being utilized to treat Major Depression at the same time. Interestingly with TMS for PTSD, a right-sided treatment target (as opposed to left-sided used in Major Depression) often provides benefit. An inhibitory vs excitatory protocol can also be tried based on response to treatment and based on specific symptoms of PTSD that are present.
-
When to pursue TMS for PTSD?
Currently, repetitive Transcranial Magnetic Stimulation-rTMS, can be considered for patients with PTSD who have not responded to or tolerated standard treatments such as:
- SSRI antidepressants or other medications.
- Talk Therapy.
It also can be a good add-on treatment option for those already receiving TMS for Major Depression. Inspire TMS Denver does not charge additional fees for add-on treatments. And our out-of-pocket rates for those seeking care outside insurance coverage are competitive. Read more: TMS therapy cost →
TMS has an excellent track record for treatment-resistant disorders such as PTSD.
TMS therapy remains a relatively new therapy only receiving FDA approval for Treatment Resistant Major Depression in 2008. However, thousands of publications and studies have taken place over the last decade-plus since then, exploring it’s benefit for other conditions such as PTSD.
-
When will I feel better?
As with TMS therapy for Major Depression, TMS therapy for PTSD follows a similar course - 5 sessions per week for 6 weeks with a 3-week taper following. Individual treatment plans may vary, however. Similarly, response times vary with TMS. Some patients experience relief from symptoms in just one to two weeks, while others take four to six weeks and may require modifications to treatment parameters and/or additional treatment sessions. More questions about TMS Therapy for PTSD or other content on this page? Please contact us here to see about a free phone consultation.
-
¹ Martin, P. The epidemiology of anxiety disorders: a review. Dialogues Clin Neurosci. 2003 Sep;5(3):281-98.
² Transcranial magnetic stimulation for post-traumatic stress disorder (nih.gov).
⁵ Repetitive transcranial magnetic stimulation in trauma-related conditions (nih.gov)
⁹https://www.sciencedirect.com/science/article/pii/S0165178118320742?via%3Dihub
TMS Therapy for Postpartum Depression
Depression Versus Celebration
The physical changes and adjustments to daily life that occur during and after pregnancy are one of the most momentous events in a woman's life. The birth of new life is a truly remarkable and humbling experience. Most associate this event with celebration and happiness and many new parents are blessed with such an experience. The stress and demands of a newborn baby and the hormonal changes that occur following birth can often result in struggles with moods, anxiety, and sleep, however. The baby blues occur commonly and can unfortunately progress on to postpartum depression.
Postpartum Depression affects some 15% of New Mothers
Pregnancy and the postpartum period can play havoc with mental health. The pressure is on new mothers to be overjoyed to bring a new life into the world, while recovering from the exhausting and painful process of giving birth. Breastfeeding can be a challenge for many and sometimes not an option due to extenuating factors or a personal decision. Most newborns don’t sleep well and need to eat every few hours as is, leading to poor sleep. Add to this an extreme change in hormone levels and it can be easy to understand how this is a high-risk time frame for postpartum depression and anxiety. Statistics point to some 15% or more of all new mothers experiencing postpartum depression each year. This approaches one million mothers per year in the US when including miscarriage and stillbirths.
¹Other general stats that are informative regarding this condition are that postpartum depression is much more common in women who have experienced depression or other mood states previously, it tends to recur with subsequent births, and there often are preclinical signs for risk of postpartum depression during the pregnancy. All of these factors speak to the importance of being proactive and planning for treatment if risk factors are present or should depressive and/or anxiety symptoms occur in pregnancy or shortly after birth. Read more: TMS therapy for anxiety →
-
What Is Postpartum Depression?
If you have struggled with depression in the past, the heightened vulnerability of pregnancy and the postpartum period can increase the likelihood for depression. For some, however, the postpartum period can be their first experience with clinical depression.
Baby blues tend to disperse after a few days as hormones rebalance and familiarity with your new baby grows and settles. Postpartum depression symptoms continue longer, however, and intensify. Postpartum depression is not drastically different from a Major Depressive Episode outside the unique factors occurring and time frame of the postpartum period. Displaying a combination of the following symptoms for more than a few days urges the need for medical consultation.
-
Symptoms of Postpartum Depression
Uncontrollable crying for lengthy periods with no apparent reason.
Recurring severe mood swings.
Irrational anxiety and worry that impedes daily life or the ability to care for the baby.
Verbalizing guilt, shame, and hopelessness.
Disclosing and radiating profound sadness and despair.
Significant lack of concentration; regularly losing and forgetting things.
Inability or avoidance of tasks and decisions
Withdrawal from partner and others
Strong reluctance to be alone with the baby - often due to fear of something bad happening to the newborn.
Apathy towards the baby, significant others, activities, and hobbies.
Lack of sleep, changes in appetite, and excessive fatigue.
Suicidal or homicidal thoughts.
Delusional, paranoid, or other psychotic thinking or hallucinations.
Postpartum depression tests are available online and if symptoms above are experienced, mental health services should be sought right away. Resources such as the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) or their web chat at suicidepreventionlifeline.org/chat are available if thoughts of suicide or psychotic symptoms occur. Additional crisis services are available through the state of CO or a mental health crisis walk-in center, or the ER in an urgent crisis. But how can we treat postpartum depression before reaching this point?
-
Transcranial Magnetic Stimulation-TMS Treatment for Postpartum Depression
A number of studies have pointed to TMS therapy as being a particularly effective treatment for postpartum depression.²³⁴⁵ These studies are relatively smaller in scale compared to the larger studies that have looked at response to TMS treatment in Treatment Resistant Major Depressive disorder, but are quite promising. Several involved lack of any medication use and the remission rates were 70-90%. The long-term response was similarly quite strong. And similar to larger studies using TMS for treatment resistant depression, the therapy was safe and well-tolerated. TMS provides an alternative to traditional treatment and the short treatment sessions (now even faster with theta-burst stimulation - read here for more about Theta Burst stimulation) can support new mothers getting back to a sense of mental wellbeing and enjoying motherhood.
-
Individualized TMS for Postpartum Depression
The team at Inspire TMS Denver offers individual consultations to explore if and how TMS could support your postpartum depression. TMS therapy offers a non-invasive and non-systemic treatment avoiding medication side effects and providing a safe treatment for mom and baby during a challenging time. If traditional treatments are not working or not an option, TMS presents a great choice for relief from depression and anxiety in the postpartum time frame. Should you elect to pursue TMS therapy for postpartum depression and associated symptoms, rest assured that Inspire TMS Denver will tailor treatment protocols to your individual symptoms and situation. More questions about TMS therapy for Postpartum depression or other information on this page? Please contact us here to see about a free consultation.
TMS Therapy for Insomnia and Sleep Disorders
Lack of sleep or low-quality sleep can test even the calmest, most tolerant personality. Chronic insomnia can trigger or worsen depressive symptoms and is also one classic symptom of both Major Depressive Disorder and Generalized Anxiety Disorder. Insomnia is also a common symptom in many other neuropsychiatric conditions.
Read more: TMS for anxiety →
Current research estimates that 30% to 40% of adults may suffer from insomnia at any given time.¹ But there’s hope. Studies are showing promising results using TMS therapy for treating insomnia, as well as for depression and anxiety disorders, which TMS is best known for.
Read more: TMS for depression →
Insomnia is typically characterized by unrelenting struggles to fall and remain asleep for an average of 6-8 hours. Inability to fall asleep in a timely fashion can be caused by, or result in, anxiety over the ability to fall asleep and a catch-22 situation occurs. When sleep does occur, it can be restless, broken, and of inadequate quality. Early wakening can occur as well and it can be impossible to get back to sleep. Daytime sleepiness, irritability, brain fog, and associated negative emotional states ensue and this significantly reduces the quality and function of daily life.
Treatment will depend on various individual factors and examination of lifestyles and medications to identify root causes. Medication or sleep medicine is usually a last resort and initial remedies should include education about sleep hygiene, avoiding stimulants such as tea and coffee, avoiding alcohol, practicing physical exercise in the daytime, setting up a regular sleep routine, ensuring a relaxing sleep environment with a cool ambient temperature, providing adequate air circulation, removing mobile phones, laptops and TVs from the bedroom and stopping use of same at least an hour before sleep. Refer to our blog post on tips for insomnia relief here →
Cognitive Behavioral Therapy-CBT is a common therapeutic tool that has proven to be effective in changing thought patterns about sleep and providing strategies for coping with anxiety related to sleep onset, middle of the night waking, and other sleep problems.
Medications can later be tried if the above does not work, but many carry high risk for dependence, tolerance, or even abuse. Hypnotics such as Ambien can cause bizarre behaviors such as sleep walking or even unconscious driving or sleep eating.
And now there is a promising new option, Transcranial Magnetic Stimulation (TMS). If the above hasn’t provided the results you’re looking for, and you don’t want the adverse effects of medications, TMS may be the answer you’ve been searching for. Transcranial Magnetic Stimulation-TMS has been shown to be very effective in resolving insomnia in several recent sleep studies. Positive effects on sleep have also been noted in other studies using TMS for treatment of other conditions - most commonly in depression and anxiety treatment.
-
Repetitive Transcranial Magnetic Stimulation-rTMS for Insomnia
During one study from 2014, after 10 days of rTMS treatment, study participants saw an improvement in total sleep time, sleep efficiency, sleep onset latency, total wake time, and wake time after sleep onset.²
Another larger study from 2013, found that rTMS improved both Slow Wave Sleep and REM sleep in comparison with CBT and hypnotic medications such as Ambien. They reported that TMS had the lowest relapse rate for insomnia and was a better long term treatment option for insomnia than CBT or medications.³
-
Treating Insomnia caused by Depression or Anxiety
TMS is most commonly known to treat Major Depressive Disorder (FDA Approved) and Generalized Anxiety Disorder (off label, but gaining traction), and while treating these disorders, a secondary effect of improved sleep and relief from insomnia is often seen. In one study, right sided rTMS treatment, typically used to treat anxiety, showed the most improvement in sleep quality with an increase in average time of sleep, decreased number of times eyes opened during sleep, and improved sympathetic activity in sleep.⁴
Read more: How TMS therapy works →
In another, Huang et al. 2018 described right sided stimulation for generalized anxiety and insomnia using a low-frequency protocol for 10 days, showing improvement in the Hamilton Rating Scale for Anxiety as well as the Pittsburgh Sleep Quality Index in 36 patients.
Another study by Li et al. 2013 studied 30 patients with major depressive disorder and 30 patients with major depressive disorder associated with insomnia receiving TMS. Both groups improved with respect to depression and the latter as well to insomnia.⁵
Another study in 2017, found TMS to the right dorsolateral prefrontal cortex improved insomnia in 20 out of 25 patients.⁶
Read more: TMS therapy for depression →
Several other studies targeting anxiety with the use of TMS likewise showed improvement in sleep parameters.⁷⁸ Other studies have similarly shown improvements in sleep parameters and quality of sleep with left sided treatment in the context of depression treatment. Measuring cortisol and melatonin levels, another case study revealed excitatory left sided treatment, which is typically used to treat depression symptoms, as effective in decreasing cortisol levels, the stress hormone, and increasing melatonin levels two days after treatment, thus resulting in improved sleep and relief from insomnia.⁹
Read more: TMS therapy for anxiety →
In a recent meta-analysis looking at multiple studies using TMS for various indications, TMS was superior to sham treatment in improving sleep efficiency, total sleep time, sleep onset latency, wake up after sleep onset, and number of awakenings.¹⁰
-
TMS for Insomnia caused by Restless Leg Syndrome (RLS)
Sleep disruption is a by-product of Restless Leg Syndrome preventing undisturbed sleep. Several studies have shown improvement in RLS and sleep with the use of TMS.¹¹¹² Improvements occurred in total sleep hours, quality of sleep, and reduction in leg movements. And benefits were sustained for at least 2 months on repeat check-in.
-
TMS for Insomnia Associated with Other Conditions
Sleep improvement has been demonstrated in several studies evaluating insomnia associated with chronic back pain, Parkinson’s Disease, and in the context of Substance Use Disorder treatment.¹³¹⁴¹⁵¹⁶
Read more: TMS vs medication →
As with other areas of neuropsychiatric research, the full use of Transcranial Magnetic Stimulation continues to be explored and insomnia symptoms have occurred in many studies. Positive developments spur further research and studies leading to improved and enhanced solutions for the myriad of neuropsychiatric conditions. As a non-invasive, and potentially fast acting treatment, how much more sleep can you afford to lose?
-
TMS for Sleep Disorder at Inspire TMS Denver
The team at Inspire TMS Denver can offer individual consultations to explore if and how TMS could support you with depression, anxiety, and insomnia. Although TMS treatment specifically for insomnia remains off-label and not covered by insurance, we offer competitive sliding scale self-payment options and insomnia often coexists in Major Depressive Disorder - which is FDA approved and insurance covered. Every contraindication will be robustly examined and if treatment is supported, the team will compose a bespoke, personalized treatment schedule catering to you and your condition. Schedule a free consultation or call us today. →
TMS Therapy for PTSD
Severe trauma engenders a range of extreme physical and psychological reactions. PTSD occurs in approximately 20% of victims of trauma and TMS may offer a return to normality.
-
What is Post Traumatic Stress Disorder?
Post Traumatic Stress Disorder-PTSD, is a psychiatric condition that follows a direct or indirect traumatic event. It typically presents with a number of problematic symptoms to be reviewed in more detail below and a chronically heightened stress state. Problems with mood and anxiety regulation occur and the mind and body struggle to reset and stay out of a fight or flight mode. Many of the symptoms of PTSD would be expected and normal in a life-threatening situation, but not in everyday life.
PTSD is most often associated with service personnel or veterans who have experienced active-duty combat and associated traumatic experiences. PTSD can occur in many other situations as well, however. Trauma can occur in small doses over many years or from one traumatic event. It can stem from things like abuse, an assault, or an accident. Some 7-9% of all people will experience PTSD in their lifetimes.¹
-
What causes PTSD?
When experiencing a real or perceived life-threatening situation, the brain will shift into ‘reptilian brain,’ prioritizing pure instinct and survival. It enters into the fight or flight mode and activates basic brain structures that keep the brain in a heightened sense of awareness and safety.
Once the threat has passed, the brain will typically down-regulate itself and return to its everyday default mode. Depending on the severity and repetitiveness of the stressful trauma, however, and the genetic predisposition of the individual, this may not occur effectively. Similar to circuits that become stuck and dysfunctional in clinical depression, certain pathways become fixed in a fight or flight response in PTSD.
-
Who is at risk of PTSD?
We all have different reactions to stressful and traumatic events and anyone can develop PTSD depending on the circumstances. Increased risk factors include:
Recurrent or longer-lasting trauma.
Suffering a physical injury or threat to life during trauma.
Lack of a support network.
Concurrent stress factors such as financial issues, homelessness, bereavement, or imprisonment.
History of depression and anxiety disorders.
Experiencing trauma in childhood.
Working in emergency services.
Refugee status.
-
Symptoms of Post Traumatic Stress Disorder - PTSD
The aftermath of a potentially life-threatening incident or repeated trauma typically manifests with natural reactions such as brief confusion, dissociation from one’s surroundings, exhaustion, a feeling of numbness, or acute anxiety or agitation. These expected reactions can support mental recovery and typically fade away. Continuing to struggle with symptoms to follow, however, indicate PTSD. PTSD symptoms have four distinct clusters:
Intrusive thoughts:
Flashbacks
Nightmares
Distressing memories.
Acute distress psychologically or physiologically at triggering reminders.
Negative mood and cognitions
Dissociative Amnesia - inability to recall aspects of the trauma.
Persistent negative emotions such as fear, anger, guilt, and/or shame.
Inability to experience positive emotions.
Feeling detached or estranged from surroundings and others.
Negativity and symptoms similar to depression such as lack of interest in activities.
Hypervigilance
Agitation and aggression.
Reckless or self-destructive behavior.
Startle response with panic attacks.
Insomnia
Difficulty concentrating.
Avoidance
Repeated effort to avoid memories or triggers related to the trauma.
Research has shown the brain actually changes biologically following traumatic experiences. Three significant brain areas become ‘dysregulated’ in PTSD:
The amygdala, responsible for recognizing and responding to threat, as well as attaching emotion to memory, becomes overactive and remains in an emergency and hypervigilant state.
The hippocampus, responsible for cells supporting neural connections that embed memory, shrinks. In reaction to the amygdala’s hypervigilance, stress hormones destroy the formation of new cells and memories that would ordinarily confirm that the threat has passed, solidifying the ‘high alert’ or reactive mode.
An area labeled the ventromedial prefrontal cortex no longer inhibits the hyperactive amygdala, thus reinforcing the inability of the hippocampus to form new memories and distinguish emotions connected to past from present.
Unsurprisingly, a combination of any of the above symptoms can severely interfere with everyday activities resulting in:
Low self-care.
Difficulties with performing and retaining a job.
Conflict in relationships and friendships.
Inability to make decisions.
Memory problems.
Struggling to deal with change.
Loss of simple joys and pleasure in life.
Inability to make decisions.
Furthermore, PTSD often occurs or causes parallel mental health issues such as:
Depression and anxiety disorders.
Suicidal ideation and/or self-harm.
Dissociative disorders.
Substance abuse.
-
Treating PTSD
Similar to other psychiatric conditions such as Major Depressive Disorder, the mainstay of treatment for PTSD involves medications and specific types of therapy. Therapy typically involves common approaches such as CBT (cognitive behavioral therapy) or more targeted therapy such as EMDR (eye movement desensitization and reprocessing), CPT (cognitive processing therapy), or exposure therapy. As is the case with Major Depression, however, PTSD treatment can often be resistant to these approaches. A recent meta-analysis showed that less than half of patients receiving trauma focused therapy achieved a meaningful response to treatment, some two-thirds of patients failed to achieve remission, and one-third dropped out of treatment. And the effect size for medications was even less than for therapy.²
TMS offers a unique approach and compelling results in the treatment of PTSD. Numerous studies have shown TMS to be an effective treatment option for PTSD when medications and therapy have not worked. Different protocols have been utilized in an attempt to treat the core symptoms of PTSD, but most, similar to depression treatment, also target an area of the brain called the dorsolateral prefrontal cortex. This area on the surface of the brain is involved in regulating deeper brain structures and can affect key areas of the brain that are involved in PTSD symptoms such as the amygdala and hippocampus.
What do the studies show?
Research has been going on for quite some time with TMS treatment for PTSD. A meta-analysis from 2014 summarized that TMS treatment for PTSD was effective and that the effect size was similar to TMS treatment for Major Depression.³ Studies reviewed included RCTs (randomized controlled studies) - the gold standard for research - and utilized validated rating scales for PTSD such as the PCL-5 (PTSD checklist) and the CAPS-5 (clinician administered PTSD scale). Some of the studies utilized as few as 10 treatments in two weeks and were found to be beneficial, but more sessions and more pulses per session tended to show greater improvement in symptoms.
More recent meta-analyses reviewing TMS treatment for PTSD have found similar and even more robust findings.⁴⁵⁶ RCTs have consistently shown at least one-third of patients with improvement on PTSD rating scales and others have been closer to one-half of patients experiencing significant response. Longer term response data is more limited, but points to at least 2-3 months of sustained response following treatment and a more recent paper has found benefit with TMS up to 1 year post treatment.⁷
In 2021, the VA implemented a nationwide study to evaluate clinical outcomes in veterans being treated with TMS.⁸ While the primary inclusion criteria for this study was Major Depression, around 68% of the patients in this study also suffered from comorbid PTSD, and both Major Depression and PTSD responses were measured. Of the 340 veterans with comorbid PTSD, 65.3% showed response and 46.1% no longer met threshold criteria after receiving an adequate dose of TMS.
Read more: TMS success rate →
Another study, which examined TMS as a monotherapy for PTSD and compared a 1 Hz protocol to a 10 Hz protocol, also found clinically significant improvements in PTSD symptoms after 30 TMS treatments.⁹ This study utilized multiple rating scales to evaluate response and remission results, and they found that around 29-46% of patients experienced response and 21-33% experienced remission (depending on rating scale). In addition to these findings, they also saw that both the 1 Hz and 10 Hz groups showed similar improvements in both PTSD and depressive symptoms, and these improvements were sustained at a 3 month follow up.
As listed above, a number of studies have shown very good results with TMS. It is not currently FDA approved for the treatment of PTSD, but often utilized off-label as PTSD can frequently be treatment resistant. As noted, other psychiatric conditions also commonly co-occur with PTSD. Major Depression occurs in some half of all PTSD sufferers. In light of this, additional treatment protocols that target PTSD more specifically can often be added into TMS being utilized to treat Major Depression at the same time. Interestingly with TMS for PTSD, a right-sided treatment target (as opposed to left-sided used in Major Depression) often provides benefit. An inhibitory vs excitatory protocol can also be tried based on response to treatment and based on specific symptoms of PTSD that are present.
-
When to pursue TMS for PTSD?
Currently, repetitive Transcranial Magnetic Stimulation-rTMS, can be considered for patients with PTSD who have not responded to or tolerated standard treatments such as:
- SSRI antidepressants or other medications.
- Talk Therapy.
It also can be a good add-on treatment option for those already receiving TMS for Major Depression. Inspire TMS Denver does not charge additional fees for add-on treatments. And our out-of-pocket rates for those seeking care outside insurance coverage are competitive. Read more: TMS therapy cost →
TMS has an excellent track record for treatment-resistant disorders such as PTSD.
TMS therapy remains a relatively new therapy only receiving FDA approval for Treatment Resistant Major Depression in 2008. However, thousands of publications and studies have taken place over the last decade-plus since then, exploring it’s benefit for other conditions such as PTSD.
-
When will I feel better?
As with TMS therapy for Major Depression, TMS therapy for PTSD follows a similar course - 5 sessions per week for 6 weeks with a 3-week taper following. Individual treatment plans may vary, however. Similarly, response times vary with TMS. Some patients experience relief from symptoms in just one to two weeks, while others take four to six weeks and may require modifications to treatment parameters and/or additional treatment sessions. More questions about TMS Therapy for PTSD or other content on this page? Please contact us here to see about a free phone consultation.
-
¹ Martin, P. The epidemiology of anxiety disorders: a review. Dialogues Clin Neurosci. 2003 Sep;5(3):281-98.
² Transcranial magnetic stimulation for post-traumatic stress disorder (nih.gov).
⁵ Repetitive transcranial magnetic stimulation in trauma-related conditions (nih.gov)
⁹https://www.sciencedirect.com/science/article/pii/S0165178118320742?via%3Dihub
TMS Therapy for Postpartum Depression
Depression Versus Celebration
The physical changes and adjustments to daily life that occur during and after pregnancy are one of the most momentous events in a woman's life. The birth of new life is a truly remarkable and humbling experience. Most associate this event with celebration and happiness and many new parents are blessed with such an experience. The stress and demands of a newborn baby and the hormonal changes that occur following birth can often result in struggles with moods, anxiety, and sleep, however. The baby blues occur commonly and can unfortunately progress on to postpartum depression.
Postpartum Depression affects some 15% of New Mothers
Pregnancy and the postpartum period can play havoc with mental health. The pressure is on new mothers to be overjoyed to bring a new life into the world, while recovering from the exhausting and painful process of giving birth. Breastfeeding can be a challenge for many and sometimes not an option due to extenuating factors or a personal decision. Most newborns don’t sleep well and need to eat every few hours as is, leading to poor sleep. Add to this an extreme change in hormone levels and it can be easy to understand how this is a high-risk time frame for postpartum depression and anxiety. Statistics point to some 15% or more of all new mothers experiencing postpartum depression each year. This approaches one million mothers per year in the US when including miscarriage and stillbirths.
¹Other general stats that are informative regarding this condition are that postpartum depression is much more common in women who have experienced depression or other mood states previously, it tends to recur with subsequent births, and there often are preclinical signs for risk of postpartum depression during the pregnancy. All of these factors speak to the importance of being proactive and planning for treatment if risk factors are present or should depressive and/or anxiety symptoms occur in pregnancy or shortly after birth. Read more: TMS therapy for anxiety →
-
What Is Postpartum Depression?
If you have struggled with depression in the past, the heightened vulnerability of pregnancy and the postpartum period can increase the likelihood for depression. For some, however, the postpartum period can be their first experience with clinical depression.
Baby blues tend to disperse after a few days as hormones rebalance and familiarity with your new baby grows and settles. Postpartum depression symptoms continue longer, however, and intensify. Postpartum depression is not drastically different from a Major Depressive Episode outside the unique factors occurring and time frame of the postpartum period. Displaying a combination of the following symptoms for more than a few days urges the need for medical consultation.
-
Symptoms of Postpartum Depression
Uncontrollable crying for lengthy periods with no apparent reason.
Recurring severe mood swings.
Irrational anxiety and worry that impedes daily life or the ability to care for the baby.
Verbalizing guilt, shame, and hopelessness.
Disclosing and radiating profound sadness and despair.
Significant lack of concentration; regularly losing and forgetting things.
Inability or avoidance of tasks and decisions
Withdrawal from partner and others
Strong reluctance to be alone with the baby - often due to fear of something bad happening to the newborn.
Apathy towards the baby, significant others, activities, and hobbies.
Lack of sleep, changes in appetite, and excessive fatigue.
Suicidal or homicidal thoughts.
Delusional, paranoid, or other psychotic thinking or hallucinations.
Postpartum depression tests are available online and if symptoms above are experienced, mental health services should be sought right away. Resources such as the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) or their web chat at suicidepreventionlifeline.org/chat are available if thoughts of suicide or psychotic symptoms occur. Additional crisis services are available through the state of CO or a mental health crisis walk-in center, or the ER in an urgent crisis. But how can we treat postpartum depression before reaching this point?
-
Transcranial Magnetic Stimulation-TMS Treatment for Postpartum Depression
A number of studies have pointed to TMS therapy as being a particularly effective treatment for postpartum depression.²³⁴⁵ These studies are relatively smaller in scale compared to the larger studies that have looked at response to TMS treatment in Treatment Resistant Major Depressive disorder, but are quite promising. Several involved lack of any medication use and the remission rates were 70-90%. The long-term response was similarly quite strong. And similar to larger studies using TMS for treatment resistant depression, the therapy was safe and well-tolerated. TMS provides an alternative to traditional treatment and the short treatment sessions (now even faster with theta-burst stimulation - read here for more about Theta Burst stimulation) can support new mothers getting back to a sense of mental wellbeing and enjoying motherhood.
-
Individualized TMS for Postpartum Depression
The team at Inspire TMS Denver offers individual consultations to explore if and how TMS could support your postpartum depression. TMS therapy offers a non-invasive and non-systemic treatment avoiding medication side effects and providing a safe treatment for mom and baby during a challenging time. If traditional treatments are not working or not an option, TMS presents a great choice for relief from depression and anxiety in the postpartum time frame. Should you elect to pursue TMS therapy for postpartum depression and associated symptoms, rest assured that Inspire TMS Denver will tailor treatment protocols to your individual symptoms and situation. More questions about TMS therapy for Postpartum depression or other information on this page? Please contact us here to see about a free consultation.
TMS Therapy for Insomnia and Sleep Disorders
Lack of sleep or low-quality sleep can test even the calmest, most tolerant personality. Chronic insomnia can trigger or worsen depressive symptoms and is also one classic symptom of both Major Depressive Disorder and Generalized Anxiety Disorder. Insomnia is also a common symptom in many other neuropsychiatric conditions.
Read more: TMS for anxiety →
Current research estimates that 30% to 40% of adults may suffer from insomnia at any given time.¹ But there’s hope. Studies are showing promising results using TMS therapy for treating insomnia, as well as for depression and anxiety disorders, which TMS is best known for.
Read more: TMS for depression →
Insomnia is typically characterized by unrelenting struggles to fall and remain asleep for an average of 6-8 hours. Inability to fall asleep in a timely fashion can be caused by, or result in, anxiety over the ability to fall asleep and a catch-22 situation occurs. When sleep does occur, it can be restless, broken, and of inadequate quality. Early wakening can occur as well and it can be impossible to get back to sleep. Daytime sleepiness, irritability, brain fog, and associated negative emotional states ensue and this significantly reduces the quality and function of daily life.
Treatment will depend on various individual factors and examination of lifestyles and medications to identify root causes. Medication or sleep medicine is usually a last resort and initial remedies should include education about sleep hygiene, avoiding stimulants such as tea and coffee, avoiding alcohol, practicing physical exercise in the daytime, setting up a regular sleep routine, ensuring a relaxing sleep environment with a cool ambient temperature, providing adequate air circulation, removing mobile phones, laptops and TVs from the bedroom and stopping use of same at least an hour before sleep. Refer to our blog post on tips for insomnia relief here →
Cognitive Behavioral Therapy-CBT is a common therapeutic tool that has proven to be effective in changing thought patterns about sleep and providing strategies for coping with anxiety related to sleep onset, middle of the night waking, and other sleep problems.
Medications can later be tried if the above does not work, but many carry high risk for dependence, tolerance, or even abuse. Hypnotics such as Ambien can cause bizarre behaviors such as sleep walking or even unconscious driving or sleep eating.
And now there is a promising new option, Transcranial Magnetic Stimulation (TMS). If the above hasn’t provided the results you’re looking for, and you don’t want the adverse effects of medications, TMS may be the answer you’ve been searching for. Transcranial Magnetic Stimulation-TMS has been shown to be very effective in resolving insomnia in several recent sleep studies. Positive effects on sleep have also been noted in other studies using TMS for treatment of other conditions - most commonly in depression and anxiety treatment.
-
Repetitive Transcranial Magnetic Stimulation-rTMS for Insomnia
During one study from 2014, after 10 days of rTMS treatment, study participants saw an improvement in total sleep time, sleep efficiency, sleep onset latency, total wake time, and wake time after sleep onset.²
Another larger study from 2013, found that rTMS improved both Slow Wave Sleep and REM sleep in comparison with CBT and hypnotic medications such as Ambien. They reported that TMS had the lowest relapse rate for insomnia and was a better long term treatment option for insomnia than CBT or medications.³
-
Treating Insomnia caused by Depression or Anxiety
TMS is most commonly known to treat Major Depressive Disorder (FDA Approved) and Generalized Anxiety Disorder (off label, but gaining traction), and while treating these disorders, a secondary effect of improved sleep and relief from insomnia is often seen. In one study, right sided rTMS treatment, typically used to treat anxiety, showed the most improvement in sleep quality with an increase in average time of sleep, decreased number of times eyes opened during sleep, and improved sympathetic activity in sleep.⁴
Read more: How TMS therapy works →
In another, Huang et al. 2018 described right sided stimulation for generalized anxiety and insomnia using a low-frequency protocol for 10 days, showing improvement in the Hamilton Rating Scale for Anxiety as well as the Pittsburgh Sleep Quality Index in 36 patients.
Another study by Li et al. 2013 studied 30 patients with major depressive disorder and 30 patients with major depressive disorder associated with insomnia receiving TMS. Both groups improved with respect to depression and the latter as well to insomnia.⁵
Another study in 2017, found TMS to the right dorsolateral prefrontal cortex improved insomnia in 20 out of 25 patients.⁶
Read more: TMS therapy for depression →
Several other studies targeting anxiety with the use of TMS likewise showed improvement in sleep parameters.⁷⁸ Other studies have similarly shown improvements in sleep parameters and quality of sleep with left sided treatment in the context of depression treatment. Measuring cortisol and melatonin levels, another case study revealed excitatory left sided treatment, which is typically used to treat depression symptoms, as effective in decreasing cortisol levels, the stress hormone, and increasing melatonin levels two days after treatment, thus resulting in improved sleep and relief from insomnia.⁹
Read more: TMS therapy for anxiety →
In a recent meta-analysis looking at multiple studies using TMS for various indications, TMS was superior to sham treatment in improving sleep efficiency, total sleep time, sleep onset latency, wake up after sleep onset, and number of awakenings.¹⁰
-
TMS for Insomnia caused by Restless Leg Syndrome (RLS)
Sleep disruption is a by-product of Restless Leg Syndrome preventing undisturbed sleep. Several studies have shown improvement in RLS and sleep with the use of TMS.¹¹¹² Improvements occurred in total sleep hours, quality of sleep, and reduction in leg movements. And benefits were sustained for at least 2 months on repeat check-in.
-
TMS for Insomnia Associated with Other Conditions
Sleep improvement has been demonstrated in several studies evaluating insomnia associated with chronic back pain, Parkinson’s Disease, and in the context of Substance Use Disorder treatment.¹³¹⁴¹⁵¹⁶
Read more: TMS vs medication →
As with other areas of neuropsychiatric research, the full use of Transcranial Magnetic Stimulation continues to be explored and insomnia symptoms have occurred in many studies. Positive developments spur further research and studies leading to improved and enhanced solutions for the myriad of neuropsychiatric conditions. As a non-invasive, and potentially fast acting treatment, how much more sleep can you afford to lose?
-
TMS for Sleep Disorder at Inspire TMS Denver
The team at Inspire TMS Denver can offer individual consultations to explore if and how TMS could support you with depression, anxiety, and insomnia. Although TMS treatment specifically for insomnia remains off-label and not covered by insurance, we offer competitive sliding scale self-payment options and insomnia often coexists in Major Depressive Disorder - which is FDA approved and insurance covered. Every contraindication will be robustly examined and if treatment is supported, the team will compose a bespoke, personalized treatment schedule catering to you and your condition. Schedule a free consultation or call us today. →


Slide title
Write your caption hereButton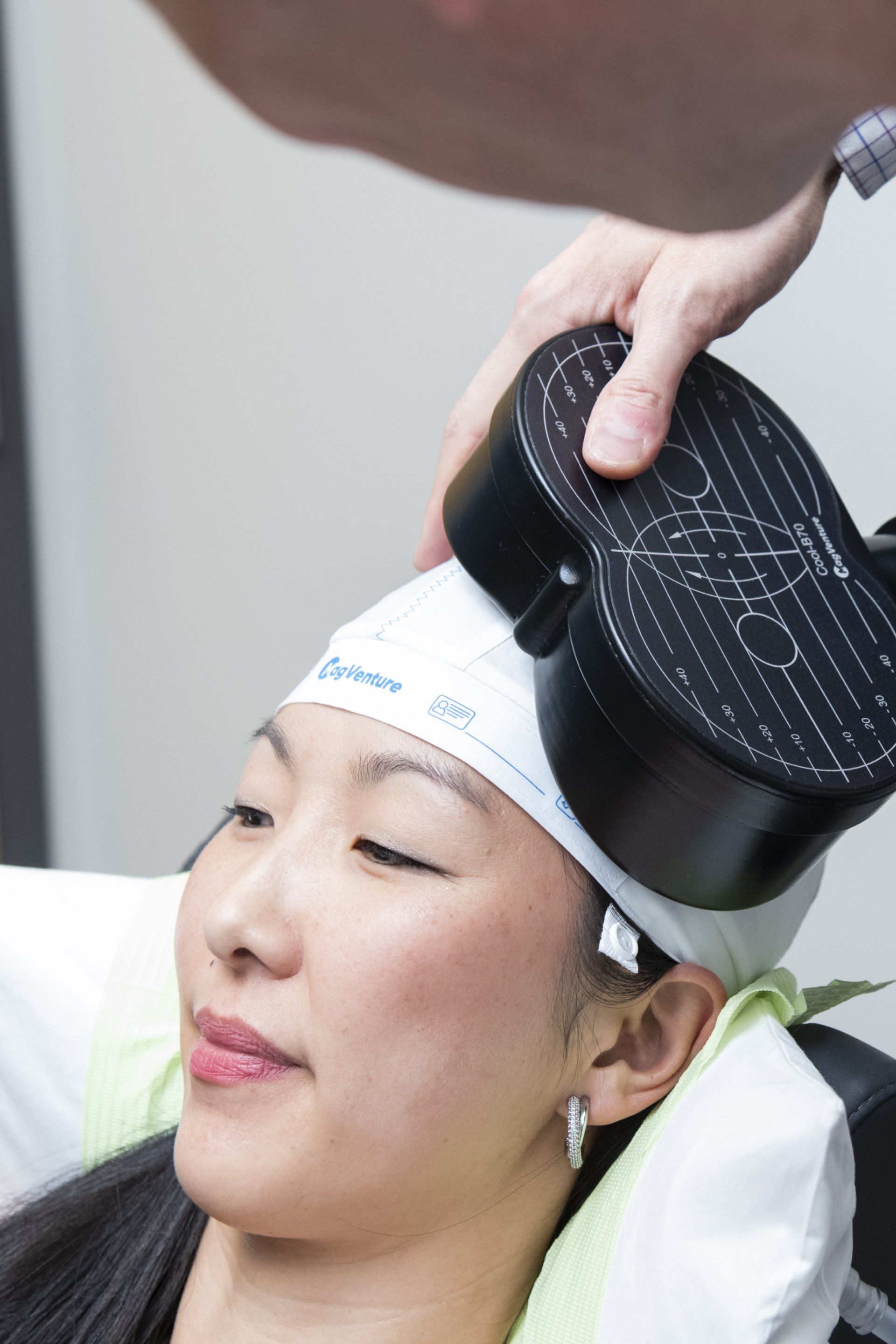
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
What Makes Us Different
Free TMS Therapy Guides, Quizzes & Phone Consultations

Patient Testimonials
Previous Patients Putting Your Mind At Rest

Amazing staff. They do a great job of explaining everything so definitely call if you’re still thinking about it. I had depression that kept me in bed for days. Since the middle of treatment I actually want to do things, and then I’m actually doing them. Completely recommend!
Communication throughout the process was absolutely excellent!! “Bedside manner” from all 3 was excellent. Office was excellent. Just cannot think of anything to critique about process from beginning to end, including pricing! Many thanks!!
the tms journey
A Step By Step Process

Book your free telephone consultation with Dr. Clinch and use this time to ask any questions or voice any concerns about TMS. If there are no contraindications to treatment, you are a good candidate, and you wish to proceed with a full evaluation, we will schedule a full intake. You will be sent an invite to our confidential patient portal and forms for review and completion that expedite care.
Shortly after this, you will be seen in person for the full TMS evaluation. This will provide adequate information for us to then submit prior authorization for TMS coverage to your insurer. If seeking care off-label through self-pay, prior authorization is not needed. We then schedule your first and all subsequent treatment sessions. We obtain prior authorization and inform you of all costs prior to starting care.
Come in for your first treatment which starts with a 'mapping' to establish your unique treatment intensity and location. Following this and at all subsequent sessions, you will recline in a motorized chair, similar to a dental visit. You can then relax, listen to music, watch TV, read or chat during the treatment. At the end of your sessions, you can drive and return to your day as normal.
Samuel B. Clinch, M.D
Medical Director
Our shared inspiration is to alleviate mental illness and improve the mental wellbeing of the patients we treat. We respect all backgrounds and cultures and want to hear our patient’s stories to best guide care. During treatment, we reinforce positive wellness practices, help maximize lifestyle modifications, and integrate rTMS therapy into a patient’s overall mental and physical health treatment.


Free Consultation
Call 720-446-8675 now, or complete the form below to request a call back.
Contact Us
We will get back to you as soon as possible.
Please try again later.
Contact Us
LOCATION
340 East 1st Avenue, Suite 333
Broomfield, CO 80020
What Happens After I Send My Message?
A member of our team will confirm your free consultation appointment within one business day.
Discover if TMS is right for you and answer all your queries about treatment, eligibility and costs.
Take the First Step Towards Your Mental Well-being Today


Slide title
Write your caption hereButton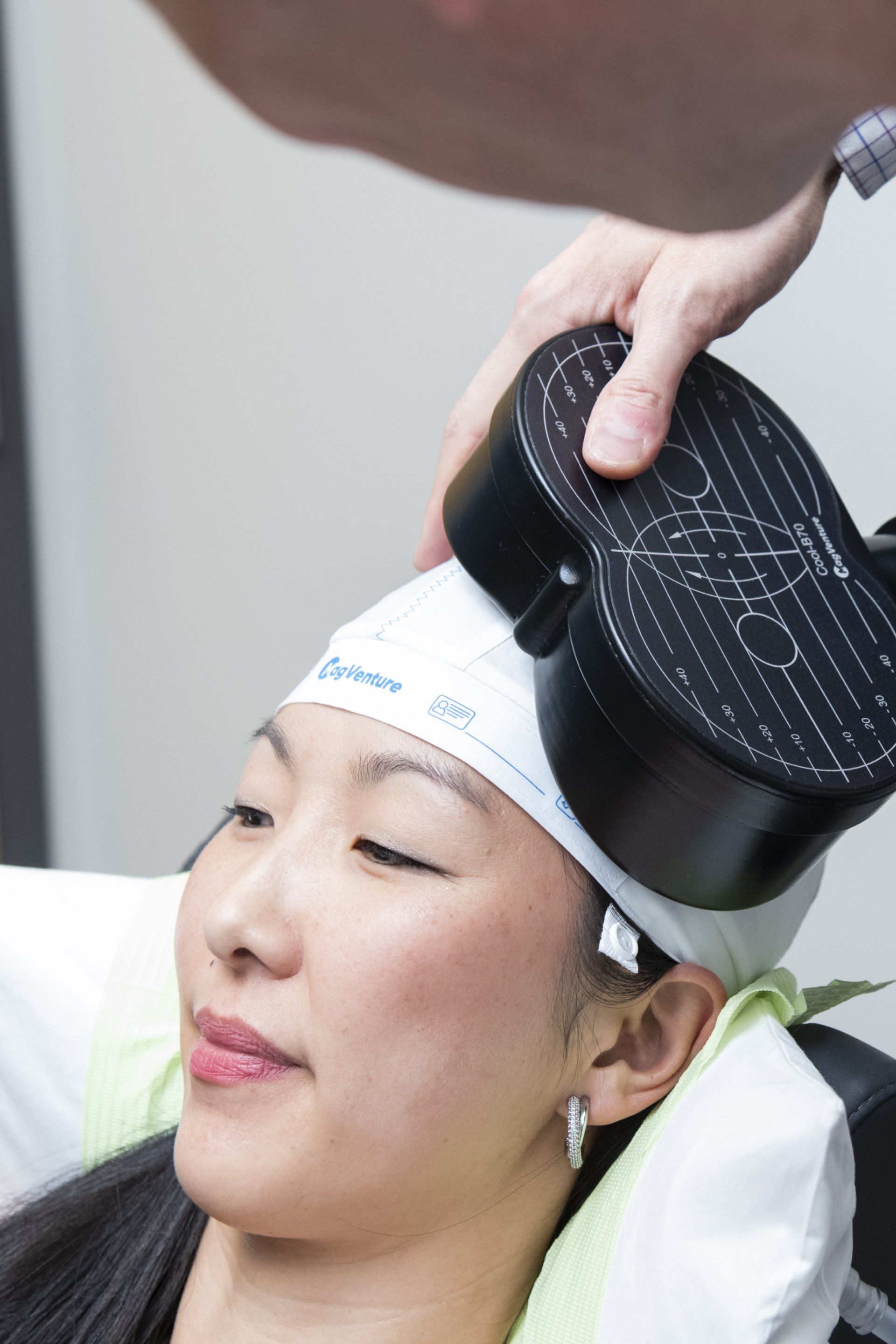
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
What Makes Us Different

Patient Testimonials
Previous Patients Putting Your Mind At Rest
I cannot say enough good things about Inspire TMS with the treatment, Dr. Clinch, and his staff. The treatment was very effective, helping me climb out of years of depression. Dr. Clinch is extremely knowledgeable, answered all my questions, and was very supportive, as was his staff.
Amazing staff. They do a great job of explaining everything so definitely call if you’re still thinking about it. I had depression that kept me in bed for days. Since the middle of treatment I actually want to do things, and then I’m actually doing them. Completely recommend!
Communication throughout the process was absolutely excellent!! “Bedside manner” from all 3 was excellent. Office was excellent. Just cannot think of anything to critique about process from beginning to end, including pricing! Many thanks!!
For more visit our Google reviews →
the tms journey
A Step By Step Process
Book your free telephone consultation with Dr. Clinch and use this time to ask any questions or voice any concerns about TMS. If there are no contraindications to treatment, you are a good candidate, and you wish to proceed with a full evaluation, we will schedule a full intake. You will be sent an invite to our confidential patient portal and forms for review and completion that expedite care.
Shortly after this, you will be seen in person for the full TMS evaluation. This will provide adequate information for us to then submit prior authorization for TMS coverage to your insurer. If seeking care off-label through self-pay, prior authorization is not needed. We then schedule your first and all subsequent treatment sessions. We obtain prior authorization and inform you of all costs prior to starting care.
Come in for your first treatment which starts with a 'mapping' to establish your unique treatment intensity and location. Following this and at all subsequent sessions, you will recline in a motorized chair, similar to a dental visit. You can then relax, listen to music, watch TV, read or chat during the treatment. At the end of your sessions, you can drive and return to your day as normal.
Our shared inspiration is to alleviate mental illness and improve the mental wellbeing of the patients we treat. We respect all backgrounds and cultures and want to hear our patient’s stories to best guide care. During treatment, we reinforce positive wellness practices, help maximize lifestyle modifications, and integrate rTMS therapy into a patient’s overall mental and physical health treatment.
Samuel B. Clinch, M.D
Medical Director
Free Consultation
Call 720-446-8675 now, or complete the form below to request a call back.
Contact Us
We will get back to you as soon as possible.
Please try again later.
Contact Us
LOCATION
340 East 1st Avenue, Suite 333
Broomfield, CO 80020
What Happens After I Send My Message?
A member of our team will confirm your free consultation appointment within one business day.
Discover if TMS is right for you and answer all your queries about treatment, eligibility and costs.
Take the First Step Towards Your Mental Well-being Today


Slide title
Write your caption hereButton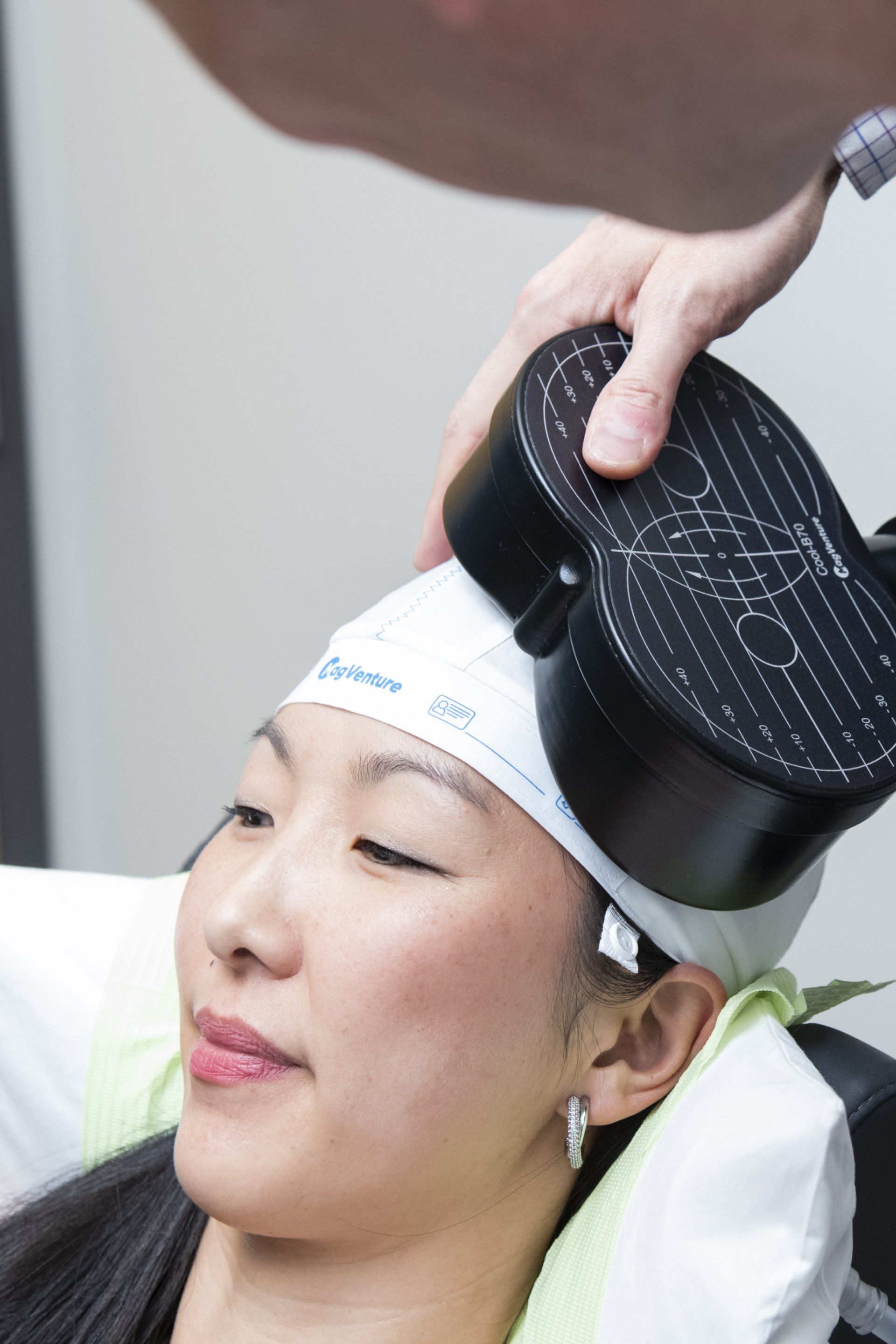
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
What Makes Us Different

Patient Testimonials
Previous Patients Putting Your Mind At Rest
I cannot say enough good things about Inspire TMS with the treatment, Dr. Clinch, and his staff. The treatment was very effective, helping me climb out of years of depression. Dr. Clinch is extremely knowledgeable, answered all my questions, and was very supportive, as was his staff.
Amazing staff. They do a great job of explaining everything so definitely call if you’re still thinking about it. I had depression that kept me in bed for days. Since the middle of treatment I actually want to do things, and then I’m actually doing them. Completely recommend!
Communication throughout the process was absolutely excellent!! “Bedside manner” from all 3 was excellent. Office was excellent. Just cannot think of anything to critique about process from beginning to end, including pricing! Many thanks!!
For more visit our Google reviews →
the tms journey
A Step By Step Process
Book your free telephone consultation with Dr. Clinch and use this time to ask any questions or voice any concerns about TMS. If there are no contraindications to treatment, you are a good candidate, and you wish to proceed with a full evaluation, we will schedule a full intake. You will be sent an invite to our confidential patient portal and forms for review and completion that expedite care.
Shortly after this, you will be seen in person for the full TMS evaluation. This will provide adequate information for us to then submit prior authorization for TMS coverage to your insurer. If seeking care off-label through self-pay, prior authorization is not needed. We then schedule your first and all subsequent treatment sessions. We obtain prior authorization and inform you of all costs prior to starting care.
Come in for your first treatment which starts with a 'mapping' to establish your unique treatment intensity and location. Following this and at all subsequent sessions, you will recline in a motorized chair, similar to a dental visit. You can then relax, listen to music, watch TV, read or chat during the treatment. At the end of your sessions, you can drive and return to your day as normal.
Our shared inspiration is to alleviate mental illness and improve the mental wellbeing of the patients we treat. We respect all backgrounds and cultures and want to hear our patient’s stories to best guide care. During treatment, we reinforce positive wellness practices, help maximize lifestyle modifications, and integrate rTMS therapy into a patient’s overall mental and physical health treatment.
Samuel B. Clinch, M.D
Medical Director
Free Consultation
Call 720-446-8675 now, or complete the form below to request a call back.
Contact Us
We will get back to you as soon as possible.
Please try again later.
Contact Us
MAIN OFFICE
720-446-8675
LOCATION
340 East 1st Avenue, Suite 333
Broomfield, CO 80020
What Happens After I Send My Message?
A member of our team will confirm your free consultation appointment within one business day.
Discover if TMS is right for you and answer all your queries about treatment, eligibility and costs.
Take the First Step Towards Your Mental Wellbeing Today
Our Services
Learning Hub
Quick Links
Our Services
Learning Hub
Quick Links
Committed
to Your Individual
Care & Recovery
Our Services
Learning Hub
Quick Links
Business Hours
- Monday
- -
- Tuesday
- -
- Wednesday
- -
- Thursday
- -
- Friday
- -
- Saturday
- Closed
- Sunday
- Closed
Find Us
LOCATION
PHONE & FAX
720-446-8675 | 720-798-6969
All Rights Reserved | Inspire TMS Denver
Information on this site is for reference purposes only. It is not intended to be nor should it be taken as medical advice. Individuals should see a medical professional regarding their symptoms.
Website by Leo Cook Digital Marketing
Committed
to Your Individual
Care & Recovery
Business Hours
- Monday
- -
- Tuesday
- -
- Wednesday
- -
- Thursday
- -
- Friday
- -
- Saturday
- Closed
- Sunday
- Closed
Find Us
LOCATION
PHONE
720-446-8675 | 720-798-6969
Information on this site is for reference purposes only. It is not intended to be nor should it be taken as medical advice. Individuals should see a medical professional regarding their symptoms.
All Rights Reserved | Inspire TMS Denver
Website by Leo Cook Marketing
Business Hours
- Monday
- -
- Tuesday
- -
- Wednesday
- -
- Thursday
- -
- Friday
- -
- Saturday
- Closed
- Sunday
- Closed
Find Us
LOCATION
PHONE & FAX
720-446-8675 | 720-798-6969
National Suicide Prevention Lifeline


Emergencies Call 911
Receive help 24 hours a day
Information on this site is for reference purposes only. It is not intended to be nor should it be taken as medical advice. Individuals should see a medical professional regarding their symptoms.
All Rights Reserved | Inspire TMS Denver
Website by Leo Cook Digital Marketing